MCW Eye reVIEW Retina Quizzes

About Dennis P. Han, MD

Retina Quiz 1: Paracentral Scotomata and Blurred Vision
Retina Quiz 2: Esotropia and Amblyopia
VA Central, steady, maintained OD; Central, steady, unmaintained OS
Anterior segment exam was normal; there was no RAPD
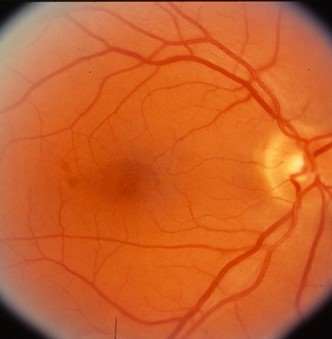
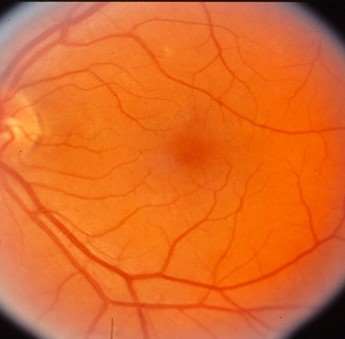
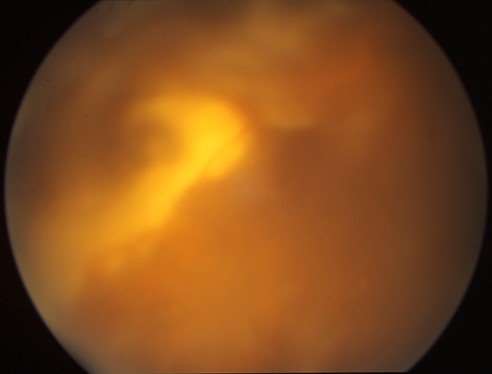
Fundus exam showed a small gray inner retinal opacity in the perifoveal region of the right eye, and a gray, flat, macular lesion in the left eye. (see images to follow)
What life threatening condition(s) might this child develop in the future?
Retina Quiz 3: Choroidal Pigmentary Abnormalities
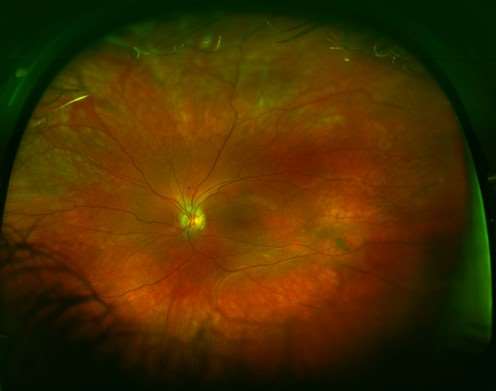
65 year old woman referred for choroidal pigmentary abnormalities RE
VA 20/100, pinhole to 20/70 RE, 20/25 LE
Right 3rd nerve palsy, corneal epithelial defects RE
History of a painful vesicular facial rash
Recent work-up for cerebral aneurysm negative
See fundus images to follow. Left fundus is normal.
What ocular condition does she have?
Retina Quiz 4: Difficulty Adapting to the Dark and Sparkles in Vision
63 year old woman with difficulty adapting to the dark and seeing sparkles in vision when going outside for the past year.
PMH: interstitial cystitis for 10 years
FH: No history of retinal degeneration or night blindness
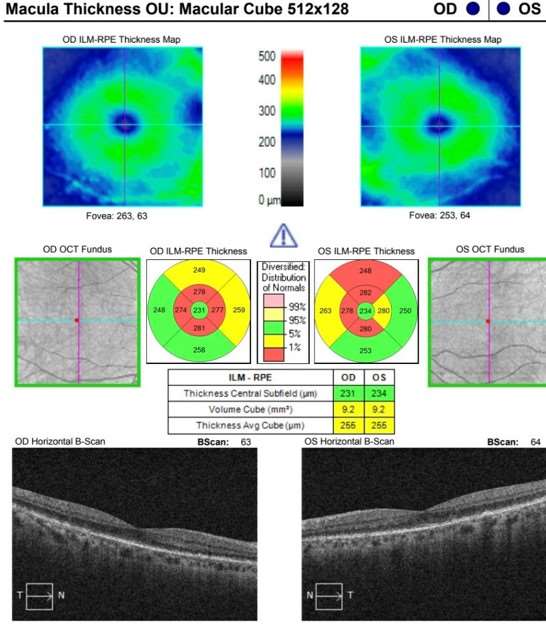
BCVA OD 20/30; OS 20/20
Confrontation visual fields full OU
Fundus exam showed diffuse pigmentary abnormality OU
See color fundus photos, fluorescein angiogram, OCT scans to follow.
What condition should you suspect? What additional imaging modality might you obtain for improved follow-up?
Retina Quiz 5: Loss of Vision Upon Awakening
59 year old woman noted loss of vision OD upon awakening
History of fevers and chills beginning 10 days prior to presentation
Had dental procedures with amoxicillin prophylaxis 9 and 6 days prior to presentation (one day after onset of fevers)
VA OD 20/400, OS 20/25
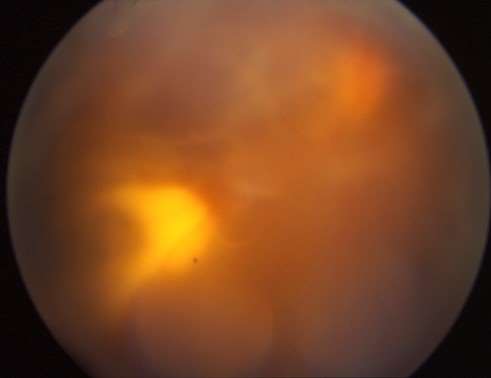
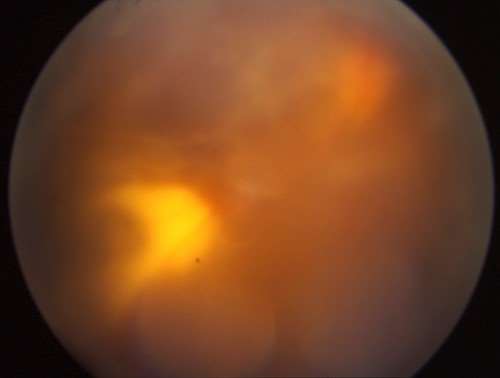
See fundus images to follow; hemorrhages present OU.
What life threatening condition might she have?
Retina Quiz 6: Juvenile X-Linked Retinoschisis
Genetic counseling
Gene therapy trials ongoing
Laser treatment indicated only to demarcate existing progressive subclinical RD with outer layer holes or full-thickness breaks
Scleral buckling or vitrectomy for clinical RD
Vitrectomy for recurrent or nonclearing VH; vitreous hemorrhages are presumed to be from perfused vessels remaining in the elevated schitic layer of the retina that have traction on them. If they break and bleed, and become completely divided, they likely will not bleed again. In recurrent cases of VH, some advocate removing the inner retinal layer(cauterizing and dividing bridging vessels) so that further traction on the vessels cannot occur. --DPH
ALL of these laser/surgical interventions are rarely needed.
Retina Quiz 7: Floaters and History of High Myopia
This 46 yr old woman complained of floaters OD for 6-7 months. Past ocular history was significant for high myopia.
Visual acuity was 20/20 OU. Anterior chamber was quiet. There were 1+ - 2+ pigmented cells in the vitreous OD. A posterior vitreous separation and peripheral operculated hole were presented OD.
No FHx of ocular lesions, eye or brain tumors, or tumors elsewhere.
What’s in your differential diagnosis?
Retina Quiz 8: Red, Painful Eye and Blurry Vision
40 y/o woman noted a red, painful right eye 10 days previously and blurry vision 2 days previously. Immigrated from Mexico 3 yrs previously. ROS negative.
VA OD 3/200; OS 20/25
Superior VF defect OD, normal OS
Slit lamp exam
OD: 1+ diffuse bulbar conj hyperemia, mild KP, 3+ AC cell, lens clear, 2+ anterior vitreous cell
OS: normal
Fundi: OD—see slides; OS—normal
Questions about our Retina Quizzes?
Email us at Ophthalmology@mcw.edu.